When should I use sterile ultrasound gel?
Here are three different scenarios in which you’ll want to use sterile ultrasound gel:- If your transducer is in contact with a mucous membrane. This effectively encompasses all transrectal and transvaginal ultrasound exams.
- If your transducer is in contact with non-intact skin.
- During surgical ultrasound scans.
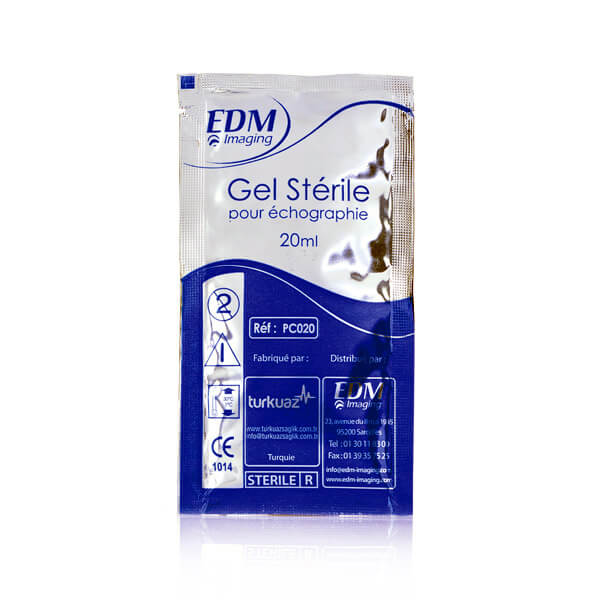 EDM Sterile Ultrasound Gel - Recommended for surgical and endocavity procedures
EDM Sterile Ultrasound Gel - Recommended for surgical and endocavity proceduresHow to use sterile gel?
The aforementioned survey from the ESR revealed that only 14% of the audited clinicians used sterile gel for their endocavity exams. From an infection control standpoint, this finding reveals a gap in the infection control practices of ultrasound users. In critical and semi-critical procedures, clinicians must measure the risk posed by every piece of equipment used during the ultrasound procedure. This includes not only the probe itself, but also the probe cover, the ultrasound gel, the cable, and the monitor. More importantly, 69% of the respondents reported that they simply wiped the probe at the end of an endocavity procedure. In effect, two thirds of the clinicians only performed low-level disinfection between each patient. Failure to perform high-level disinfection fosters pathogenic transmission via the ultrasound probe, and subsequently, the gel container (if single-use packets are not employed). Healthcare-associated infections in ultrasound procedures can spread by missing just one step. Consider this scenario: an exam is performed on an infected patient, the probe cover fails and the probe becomes infected, the probe is simply wiped down but does not undergo high-level disinfection, and thus the gel bottle is infected when applied to the infected probe during the next procedure. The next patient is then infected when the probe and gel are used on him/her. Parker Aquasonic - sterile ultrasound gel
Parker Aquasonic - sterile ultrasound gel- Use sterile ultrasound gel for endocavity procedures. We recommend the single-use packets as they are discarded and eliminate the risk of cross-contamination.
- Use a new refill bottle on a regular basis for your non-critical, surface ultrasounds (on intact skin).






