Our infection control solutions
From probe covers to high-level disinfection, we have what you need to keep your patients safe.
Learn more
Your Role in Infection Prevention
When it comes to patient safety, healthcare providers like you can act as guardians against invisible threats. Every day, you wield expertise and compassion to safeguard those in your care. With the rise of healthcare-associated infections (HAIs), your role extends beyond treatment—it encompasses proactive infection prevention.
The battle against infections demands diligence and requires a strategy built on robust practices, continual education, and a deep commitment to excellence. Statistics reveal a grim reality, with 1 in 31 hospital patients contracting at least one HAI on any given day. But together, we can change this narrative.
Here are 4 areas that are a part of actively engaging in the battle against healthcare-associated infections:
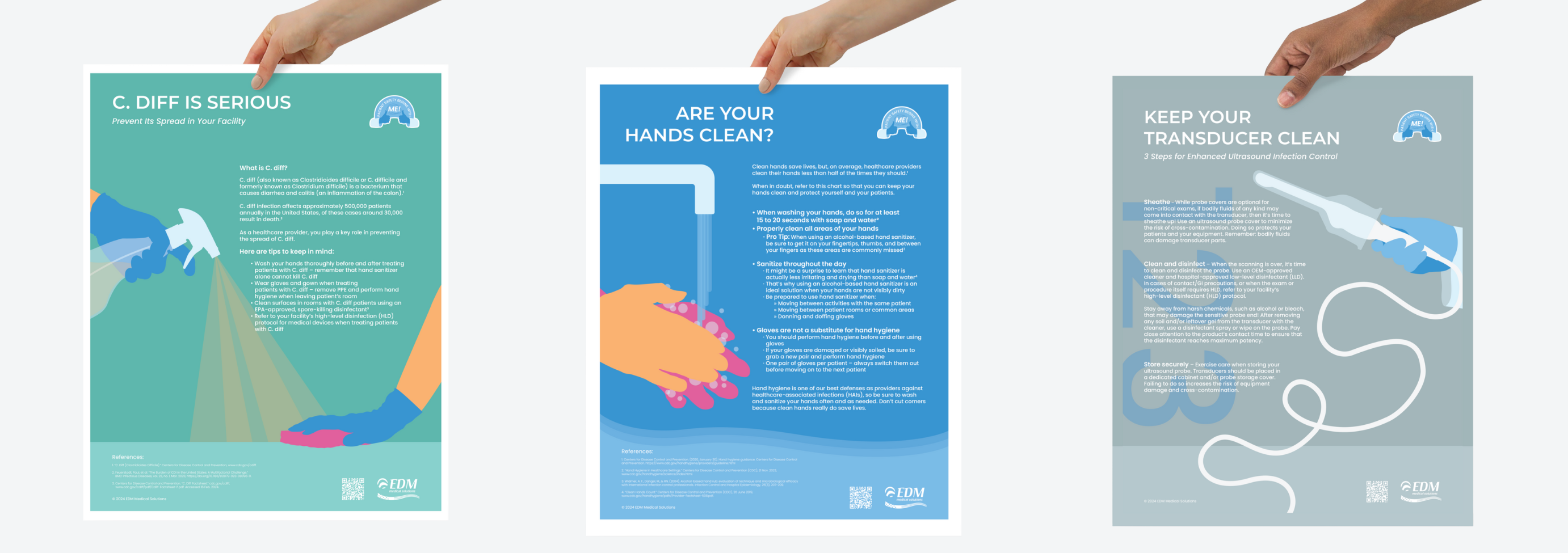
Hand Hygiene
Proper hand hygiene is crucial for healthcare practitioners to minimize infection risks. From ultrasound technicians to nurses, direct patient contact is common across medical specialties. Failing to wash hands properly can lead to pathogen transmission, endangering both patients and clinicians.
The CDC highlights the effectiveness of hand washing in preventing the spread of antibiotic-resistant germs. Whether touching patients, nearby surfaces, or medical devices, a thorough 15-second minimum hand wash is imperative.
Five critical moments for hand washing include before aseptic procedures, after exposure to bodily fluids, post-physical assessments, upon entering patient areas, and before leaving, even if no direct contact occurred.
Proper Glove Use
Medical gloves serve as a protective barrier against infectious pathogens, as advised by the CDC for situations involving potential exposure to bodily fluids or contaminated surfaces. However, it's vital to understand that gloves do not replace proper hand washing.
Healthcare providers should wash and/or sanitize their hands before and after glove use to ensure thorough hygiene. Additionally, selecting the appropriate glove type—sterile or non-sterile, latex or latex-free—is important and should align with the facility's infection prevention guidelines.
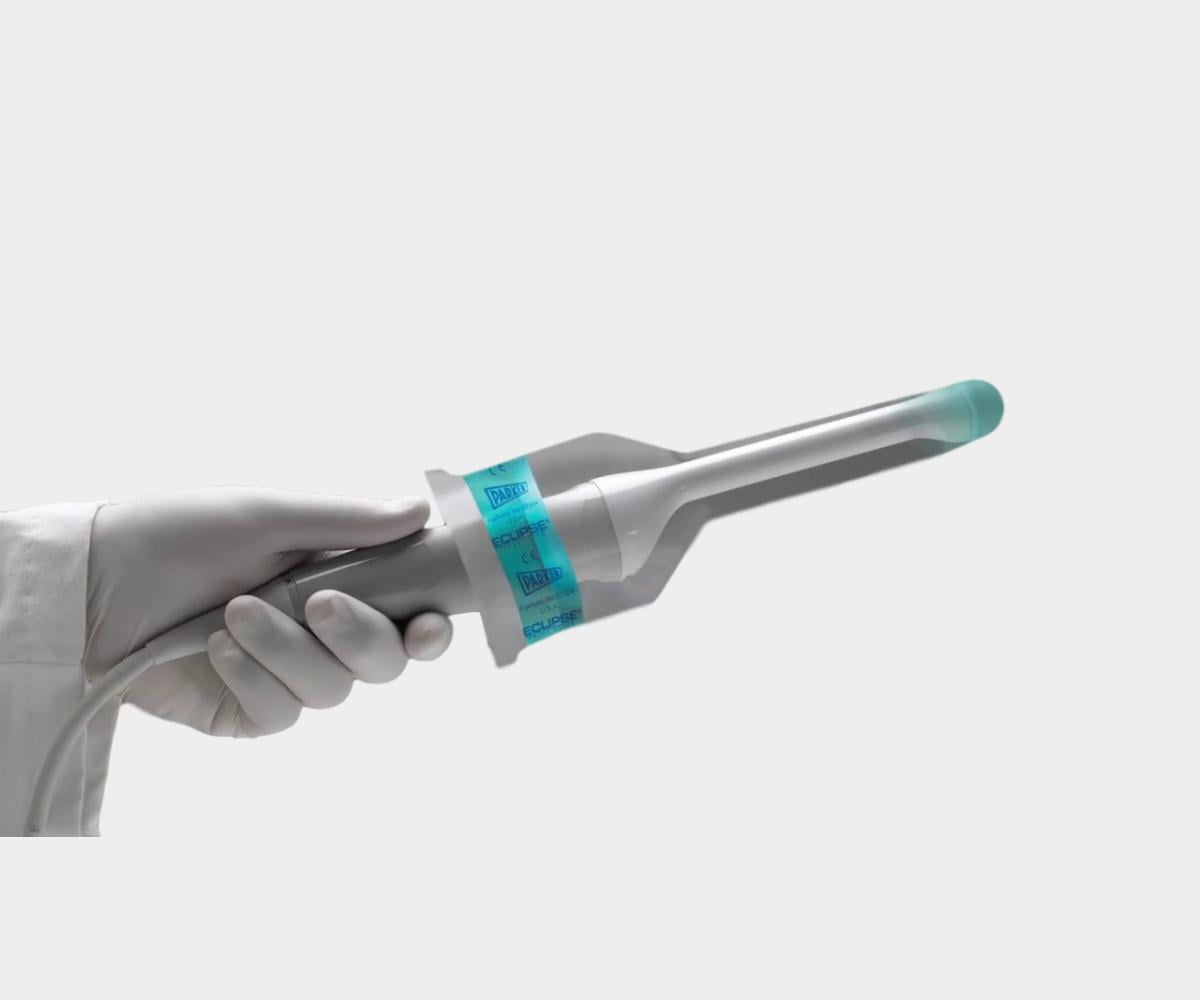
Ultrasound Transducer Sheathing & Disinfection
Ultrasound is now used for a variety of surgical or perioperative applications such as nerve blocks, TEE cardiac monitoring, Vascular access (CVC placement), Intracranial Pressure (ICP) assessment, and more.
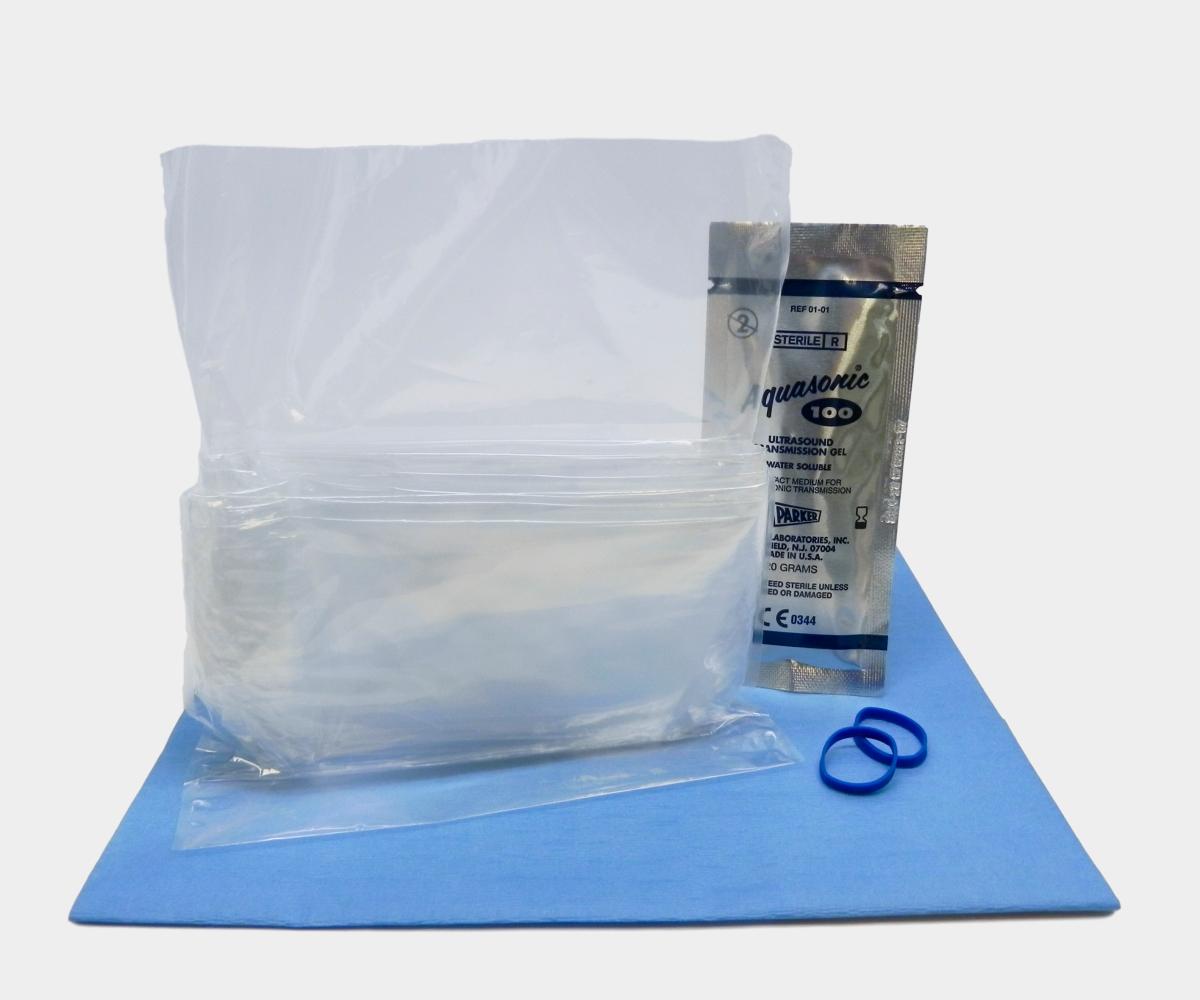
When ultrasound imaging is used in a sterile environment such as the operating room, the equipment must be covered with a sterile sheath to maintain the sterile field, and only sterile gel is recommended both inside and outside the probe cover.
To reduce the risk of spreading healthcare-associated infections, imaging staff should clean and disinfect the probe, use a probe cover, and apply a sterile gel. These recommendations, however, are contingent upon the nature of the procedure as described above and are therefore subject to change.
Surface ultrasound on intact skin for diagnostic purposes
· No need for a cover
· No need for sterile gel
· Cleaning and low-level disinfection is sufficient
Surface ultrasound for intervention
· Need for sterile cover
· Need for sterile gel
· Need for high-level disinfection after each patient use
Endocavity for diagnostic purposes
· Need for a probe cover (non-sterile is accepted, but we highly recommend sterile)
· No need for sterile gel, but we highly recommend sterile
· Need for high-level disinfection (or sterilization if possible) after each patient use
Endocavity intervention (such as a biopsy or IVF procedure)
· Need for sterile cover
· Need for sterile gel
· Need for high-level disinfection (or sterilization if possible) after each patient
Clean and Disinfect Surfaces
Healthcare practitioners, especially those in interventional settings, should adhere to facility infection control protocols and use appropriate disinfectants for devices.
High-risk environments, like surgical or interventional settings, may require elevated disinfection levels, such as the use of high-level disinfection for endocavity ultrasound transducers post-patient use.
Collaboration with the infection control department is essential for determining proper reprocessing based on procedure nature and supplies used.
Inadequately reprocessed devices pose a significant infection risk to other patients. Prioritizing infection prevention, as highlighted by the CDC, can substantially reduce healthcare-associated infections.
It is important to note how medical practices should use a 6-log kill rate to ensure the highest level of disinfection possible. The logarithmic scale provides a way to measure log reductions, or the decrease of pathogens, by working with factors of 10.
According to the EPA, log reduction as a percentage reduction can be measured this way:
· 1-log reduction = 90% reduction
· 2-log reduction = 99% reduction
· 3-log reduction = 99.9% reduction
· 4-log reduction = 99.99% reduction
· 5-log reduction = 99.999% reduction
· 6-log reduction = 99.9999% reduction
This concept can be better visualized when applied to a colony of one million C. diff bacteria. The kill rates are as follows:
· A 1-log kill reduces the colony to 100,000 C. diff bacteria
· A 2-log kill reduces to 10,000 C. diff bacteria
· A 3-log kill reduces to 1,000 C. diff bacteria
· A 4-log kill reduces to 100 C. diff bacteria
· A 5-log kill reduces to 10 C. diff bacteria
· A 6-log kill reduces to 1 C. diff bacteria
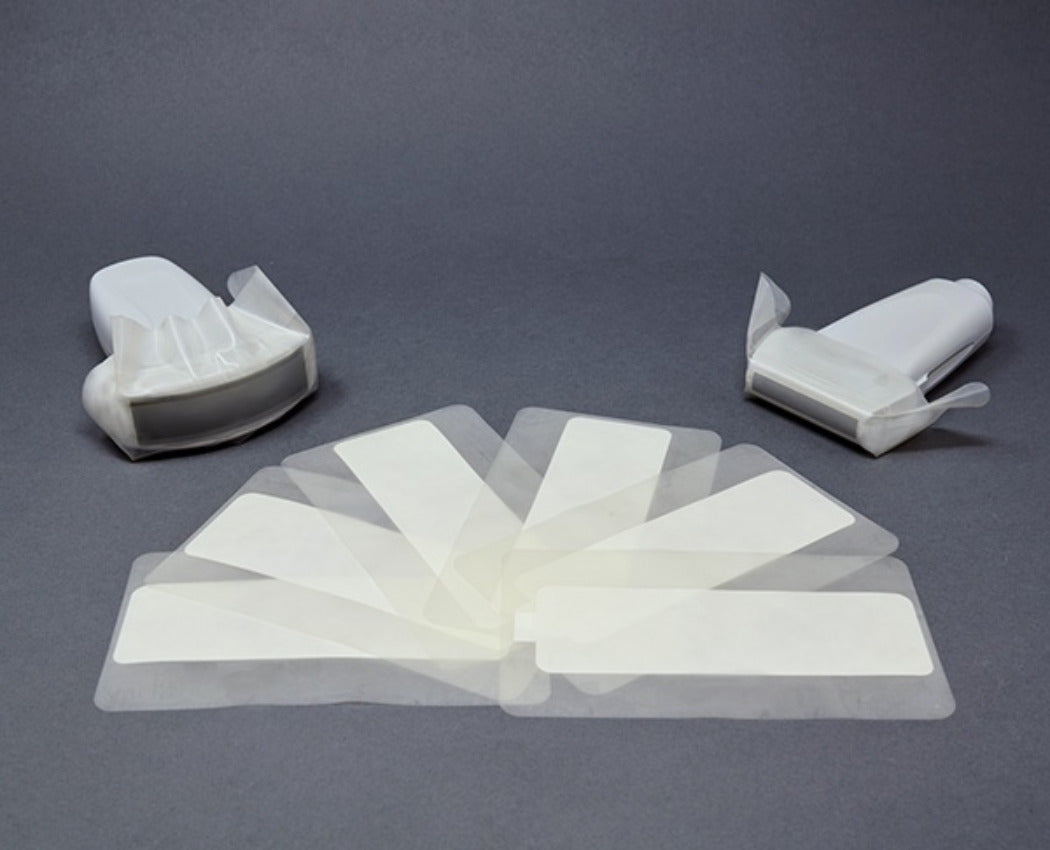
Medical equipment, including imaging devices such as ultrasound transducers, c-arm scanners, and others, should be properly cleaned and disinfected. Depending on the imaging device, some may require cleaning and disinfecting after each patient use, such as endocavity ultrasound transducers.
In addition, certain devices should be stored to preserve their cleanliness and prevent cross-contamination, such as ultrasound probes which can be safely stored in storage covers.

How We Can Improve Infection Control Practices
Insights into key steps you can take to keep patients safer and improve outcomes
Partner with infection control specialists
Collaborate with infection control experts to assess and enhance protocols, whether through internal departments or external consultants. Stay informed by joining organizations like APIC and attending seminars to stay updated on infection control methods and trends.
Establish a culture of infection control
Foster a culture of infection control where every staff member recognizes their role in preventing infections, shifting from viewing it as solely the responsibility of specialists to a collective effort within the healthcare facility. Educate visitors on infection control practices to minimize risks of contamination.
Adhere to recognized practice standards
Adhere to accepted standards of practice, regularly monitoring equipment like autoclaves and ensuring compliance with state, federal, and facility-specific guidelines outlined by the CDC.
Ensure staff competency and oversight
Provide ongoing training and education on infection control for staff, documenting their participation and periodically reviewing protocols to reinforce their importance in reducing healthcare-associated infections.