The recent release of the final rule for the Calendar Year (CY) 2024 Hospital Outpatient Prospective Payment System (OPPS) and Ambulatory Surgical Center (ASC) payment rates by the Centers for Medicare & Medicaid Services (CMS) has significant implications for healthcare providers and ambulatory surgery centers. This comprehensive rule encompasses various adjustments to payment rates, reflecting CMS's ongoing commitment to equitable reimbursement structures and the promotion of quality care delivery.
A Closer Look
One of the central aspects of the final rule is the adjustment to both OPPS and ASC payment rates, featuring a notable increase of 3.1%. This increase, which surpasses the initially proposed 2.8% rise, is based on a market basket increase of 3.3%, with a 0.2 percentage point reduction for productivity adjustment.
Amid public concerns raised during the comment period about the sufficiency of the proposed rate increase, CMS justified its decision by referencing a statutory requirement for aligning the outpatient department fee schedule increase factor with the inpatient payment system market basket percentage increase factor.
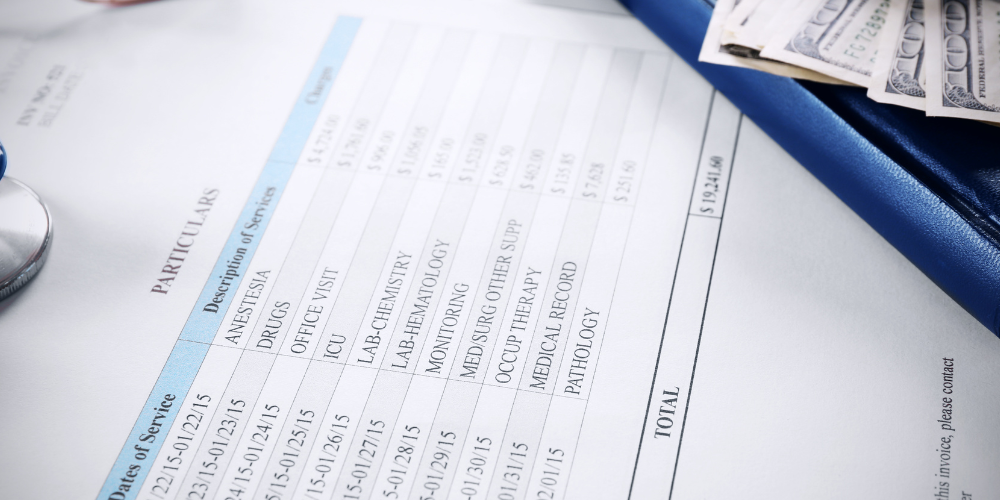
Payment Changes
The finalized payment rates hold implications for hospitals and ASCs, particularly concerning their adherence to outpatient quality reporting (OQR) requirements. Non-compliant facilities face a 2% reduction in payment rates, with the OPPS conversion factor set at $87.382 (or $85.687 for non-compliant hospitals) and the ASC conversion factor at $53.514 (or $52.476 for non-compliant ASCs). Notably, CMS estimates that total payments to OPPS providers are projected to increase by approximately $6 billion over CY 2023, with ASC payments expected to rise by $207 million.
Regional and Specialty Variations
The impact of these payment rate changes varies across different healthcare settings and specialties. Urban hospitals can anticipate a 3.2% increase in payments, while rural hospitals are poised for a 4.2% increase. Furthermore, nonteaching hospitals are expected to see a 3.9% rise, with minor and major teaching hospitals experiencing 3.5% and 2.4% increases, respectively. Surgical specialties may experience varying levels of payment fluctuations due to ASC provisions in the final rule, indicating potential impacts on specific medical services and procedures.

Additions to the ASC-CPL
CMS has made significant additions to the ASC Covered Procedures List (ASC-CPL), finalizing the inclusion of 37 surgical procedures aimed at enhancing access to outpatient surgical care and streamlining healthcare delivery. Among these additions are 26 dental codes, as initially proposed, alongside 11 additional surgical codes covering a spectrum of procedures. These procedures encompass various reconstructive surgeries for areas like the jaw, shoulder, and ankle, as well as interventions such as tendon incision and vena cava filtration.
Notably, total shoulder arthroplasty is among the procedures added. ASCA Chief Executive Officer Bill Prentice commends CMS for this decision, emphasizing the benefits for Medicare beneficiaries in terms of affordability and the potential cost savings for the Medicare program.
Additionally, CMS has extended the alignment of the ASC update factor with that used for updating HOPD payments, continuing the five-year interim period for an additional two calendar years through 2025.
Overall, CMS's final rule for CY 2024 marks a crucial advancement in healthcare reimbursement and quality care delivery. With payment rate adjustments, alignment extensions, and additions to the ASC-CPL, CMS demonstrates its commitment to enhancing accessibility and efficiency in outpatient surgical care, benefiting providers and patients alike.