In a recent issue of the RSNA’s journal, Radiology, a special report outlined the prevention, diagnosis, and treatment of complications stemming from blood clots in COVID-19 patients. In addition, the journal published two research letters and a case study on the topic.
As COVID-19 spreads throughout the world, clinicians have been forced to face the virus with no proven treatment options. Physicians combatting the respiratory virus have utilized diagnostic imaging, such as ultrasound and CT, as they attempt a variety of different treatment options and tailor their approach on a case-by-case basis.
Due to recent reports that have demonstrated a strong association between elevated D-dimer levels and poor prognosis, concerns have risen about thrombotic complications in COVID-19 cases.
In response, the National Institute for Public Health of the Netherlands requested that a group of radiology and vascular medicine experts provide guidance for the treatment of these complications. The group produced a report which summarizes evidence for thromboembolic disease as well as the potential preventative and diagnostic action that clinicians can take.
“Worldwide, COVID-19 is being treated as a primary pulmonary disease,” said Edwin J.R. van Beek, M.D., Ph.D., director at Edinburgh Imaging, Queens Medical Research Institute, at the University of Edinburgh, U.K. “From the analysis of all available current medical, laboratory and imaging data on COVID-19, it became clear that symptoms and diagnostic tests could not be explained by impaired pulmonary ventilation alone.”

Researchers have observed that respiratory failure in COVID-19 patients is not only caused by the development of the acute respiratory distress syndrome. Their observations suggest that microvascular thrombotic processes may play a role as well. There is a strong association between D-dimer levels, disease progression, and chest CT features pointing to venous thrombosis. These findings may signify important consequences for the diagnostic and therapeutic management of these cases.
Moreover, multiple studies involving COVID-19 patients have revealed a correlation between increased D-dimer levels and severe disease. The authors of the special report stress that careful attention must be paid to the initial diagnosis and treatment of the prothrombotic and thrombotic state that can occur in cases of the virus.
“Imaging and pathological investigations confirmed the COVID-19 syndrome is a thrombo-inflammatory process that initially affects lung perfusion, but consecutively affects all organs of the body,” Dr. van Beek said. “This highly thrombotic syndrome leads to macro-thrombosis and embolism. Therefore, strict thrombosis prophylaxis, close laboratory and appropriate imaging monitoring with early anti-coagulant therapy in case of suspected venous thromboembolism are indicated.”
The recommendations for therapeutic and diagnostic management in COVID-19 cases include prophylactic-dose heparin, CT pulmonary angiography, chest CT, and routine D-dimer testing. It is important to note, however, that these vary significantly on the basis of patient symptoms and risk profiles.
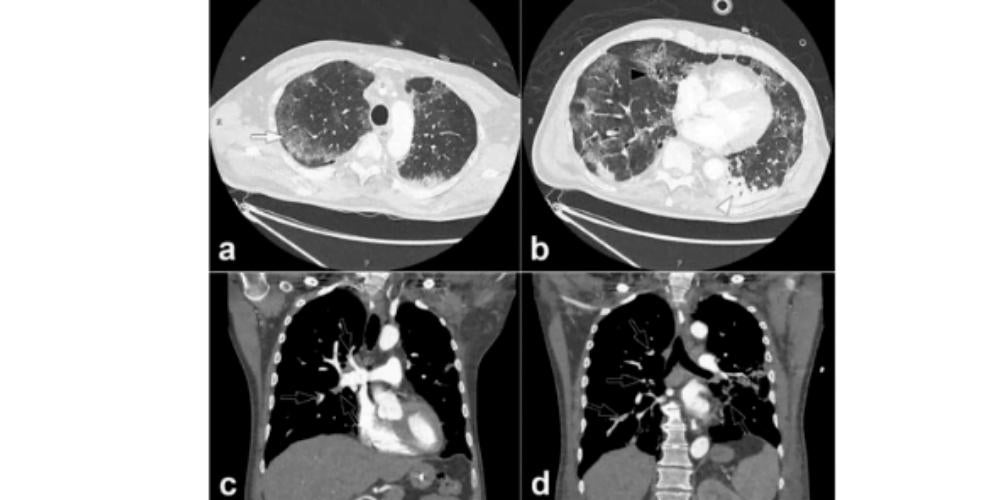
Furthermore, findings have also come to light linking COVID-19 to pulmonary embolism. In a research letter from Hôpitaux Universitaires de Strasbourg published in Radiology, the authors reported that of 106 pulmonary CT angiograms performed for COVID-19 patients over a one-month period in a tertiary care center in France, 32 patients (30%) experienced acute pulmonary embolus (PE). The rate of PE experienced by these patients was much higher than has been typically encountered in critically ill patients without the virus (1.3%), or in ER patients (3% to 10%). In this study, a D-dimer threshold of 2660 μg/L detected all patients experiencing pulmonary embolus on chest CT.
In another research letter from Centre Hospitalier Universitaire de Besancon in France, a study found that a higher proportion of COVID-19 patients had PE when contrast CT was used as the diagnostic imaging method. From symptom onset, PE was diagnosed at mean of 12 days. In addition, these patients with PE were more likely to need care in the critical care unit and be placed on mechanical ventilation.
In a case report from Cooper University Hospital in Camden, NJ, researchers described multiple areas of arterial and pulmonary thrombosis in an 84 year old male COVID-19 patient.
“COVID-19 is more than a lung infection,” Dr. van Beek said. “It affects the vasculature of the lungs and other organs and has a high thrombosis risk with acute life-threatening events that require adequate treatment with anticoagulants based on laboratory monitoring with appropriate imaging tests as required.”