Methicillin-resistant Staphylococcus aureus, referred to commonly as MRSA, poses a serious threat to patients during their stay in healthcare facilities. This antibiotic-resistant bacteria is a dangerous strain of Staph that can lead to health complications. MRSA’s resistance to the most used antibiotics makes it a formidable foe in the fight against healthcare associated infections.
Both healthcare providers and administrators are asking themselves, “which infection control measures are important for MRSA?” While the recent pandemic has forced many hospitals and smaller healthcare facilities to shift their resources in the fight against COVID-19, clinicians must remain alert and aware of the threat that other healthcare-associated infections pose. The battle against HAIs continues to be fought on several fronts and MRSA has not stopped frustrating some healthcare practitioners and the infection preventionists who support them.
The key in the fight against MRSA is prevention. Infection prevention, when applied appropriately, can prevent a patient or a member of the medical staff from ever contracting the bacteria in the first place. Keeping all stakeholders in the facility as well as patients healthy and free from healthcare-associated infections is the goal, after all. Thus, it is crucial that we look at which infection control measures clinicians can take to prevent the spread of MRSA.
From 2005 to 2014, the Centers for Disease Control and Prevention (CDC) reported that the overall estimated incidence of invasive MRSA infections from sterile sites, such as blood and pleural fluid, in the United States saw a decline of 40%. Moreover, during the same time period, the CDC reported that the incidence of invasive hospital-onset MRSA infections declined by 65%. Much of this decline is attributed to infection control interventions, such as contact precautions, disinfection, and hand hygiene, which have reduced the risk of MRSA spread.
In recent decades, studies have suggested that the spread of non-endemic MRSA can not only be contained but also eradicated in certain situations, as was seen in Finland in the early 1990s and where MRSA is now largely confined to long-term care facilities rather than acute hospitals. However, the question of whether it is possible to eradicate MRSA in hospitals or clinics where it is endemic is debated among infection preventionists. Regardless, clinicians should know that even in situations where MRSA is endemic, it is possible to control the spread of the disease and minimize its impact on patient safety.
Protecting patients from MRSA, and any other healthcare-associated infection, cannot be done without a strategy. Infection prevention and control protocols that are effective and have successful results can only be carried out when there are clear guidelines in place to combat the disease in question. As a result, the CDC as well as other organizations have issued a variety of infection control guidelines related to MRSA over several years.
In this article, we will cover three key aspects of MRSA infection control: surveillance, disinfection, and hand hygiene.
Surveillance
Forming a key aspect of infection control, surveillance must be considered in any infection control program, especially one for MRSA. This is the instrument which infection preventionists and clinicians can use for early detection and proper threat assessment. With an effective surveillance program in place, healthcare facilities will be aware of any changes in patterns of infection, thus allowing them to better quantify the problem. It also allows practitioners and administrators to monitor trends and compare rates, evaluate the efficacy of infection control interventions, reinforce good practices, and identify areas in need of further investigation.
Surveillance itself should be viewed as an infection control intervention. By appropriately looking out for spikes or abnormalities in infection rates, healthcare facilities can better prepare for the potential of a MRSA outbreak. It allows clinicians to identify areas where the outbreak may stem from and give them the opportunity to prevent the spread of the disease before it’s too late.
Disinfection
The disinfection of surfaces in the patient environment as well as medical devices is an important aspect of MRSA infection control. However, medical staff should be well aware that not all disinfectants are able to combat the same diseases. In healthcare settings, especially hospitals, facilities should opt to use hospital-grade disinfectants capable of killing a wide range of healthcare-associated infections such as MRSA.
While there may be a wide variety of disinfectants for clinicians to choose from, it is important to take into consideration the goals of the disinfection. Clinicians should ask themselves questions like, “what pathogens should I focus on in this setting?” and, “what is the most convenient format to perform the disinfection?” Selecting a disinfectant should be given good thought to ensure that is the most effective option.

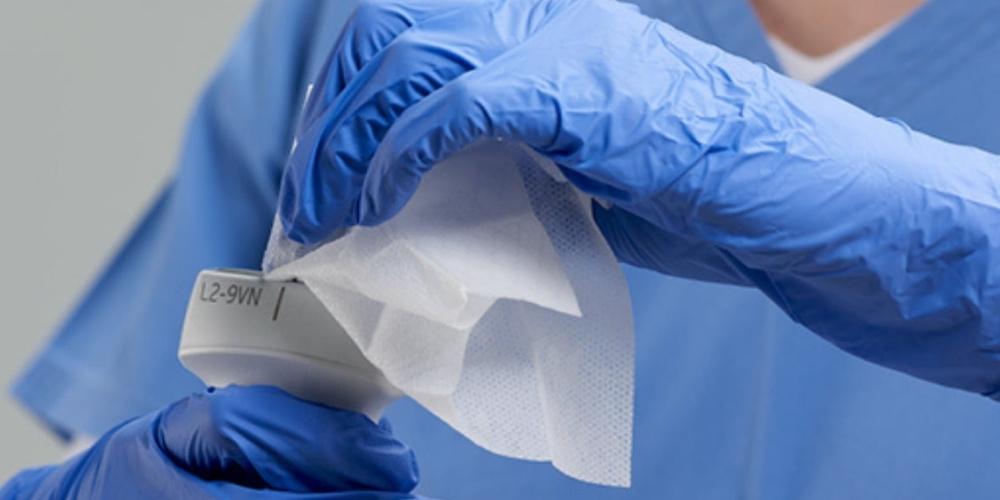
Medical staff can choose between disinfectant wipes and sprays. One is not necessarily more effective than the other: it depends on the solution which the spray or wipe contains. The Protex disinfectant from Parker Laboratories comes in both a spray and a wipe. This convenient disinfectant kills MRSA plus over 47 different other pathogens. Disinfectants such as these are an ideal choice for facilities with the need to disinfect not just surfaces, but medical devices as well because they will not damage the device.
Another top choice for medical professionals are SONO disinfecting wipes. SONO wipes begin killing on contact and eliminate 99.9% of bacteria in just 15 seconds. They are also effective against MRSA and are safe to use on a variety of medical devices, including ultrasound transducers. It is important to disinfect the patient environment as well as any medical devices which he or she may come into contact with.

By properly disinfecting the area, clinicians can more effectively reduce the risk of surface-to-patient transmission of MRSA. However, not all disinfectants are effective against MRSA. Be sure to check with the disinfectant manufacturer and verify that it is capable of combatting MRSA. It is advisable to opt for higher levels of protection, such as those offered by Parker Protex disinfectant spray and wipes and SONO disinfecting wipes, which can reduce the risk of a wide variety of healthcare-acquired infections including MRSA as well as work on multiple surfaces, including sensitive ones like ultrasound probes.
Hand Hygiene
Clinicians must not neglect hand hygiene when working in a medical setting. It is of the utmost importance that all healthcare workers be aware of the risk which unclean hands pose to patients as well as other staff members. Hand hygiene is the very first action which clinicians should take to increase patient safety.
Healthcare facilities should ensure that their infection control protocols give clear instructions on how clinicians must properly wash their hands. In addition, informing healthcare providers on the why behind hand hygiene is equally important. Infection preventionists must view their role as educators, and as a result, the facility’s infection control protocols should properly inform clinicians of the risk of failing to comply.
Studies have found that adhering to hand hygiene protocols in a strict fashion can reduce the spread of pathogens, including the propagation of MRSA in hospital settings. For patient who have contact precautions, staff members should take extra care to ensure that not just staff but also family members and loved ones take care in adhering to proper hand hygiene. While the unclean hands of a clinician are a threat to patient safety, we must not forget that the unclean hands of visitors pose a significant threat as well.
All stakeholders in the healthcare facility as well as visitors should be informed and encouraged to follow proper hand hygiene. Doing so is a step towards minimizing the risk of MRSA spread in high-risk medical settings.
EDM offers a range of comprehensive solutions for infection control. Learn more about our process driven approach to infection prevention and control here.