Physicians have found that pneumonia induced by COVID-19 typically worsens between one and two weeks of symptom onset. Therefore, practitioners have been using medical imaging to aid in monitoring patients and predicting their need for oxygen and ventilation. The timing and use of the imaging must be precise, according to French thoracic imaging specialist Professor Antoine Khalil.
In a recent European Society of Cardiology (ESC) webinar, Khalil stressed how patients should not be imaged without proper cause as this can increase the risk of infecting technicians and other staff who may be exposed to contamination. He encouraged medicals staff to be conservative in their use of diagnostic imaging when it came to suspected COVID-19 cases.
Khalil, who is also the head of radiology at Hôpital Bichat-Claude Bernard in Paris and president of the French Society of Thoracic Imaging, shared the following advice with viewers:
- Unless the patient is hospitalized or needs oxygen, do not perform diagnostic imaging. This increases the risk of exposing technicians and other staff in the facility.
- Opt for CT over x-ray if possible. This is another way to limit the staff’s exposure to COVID-19.
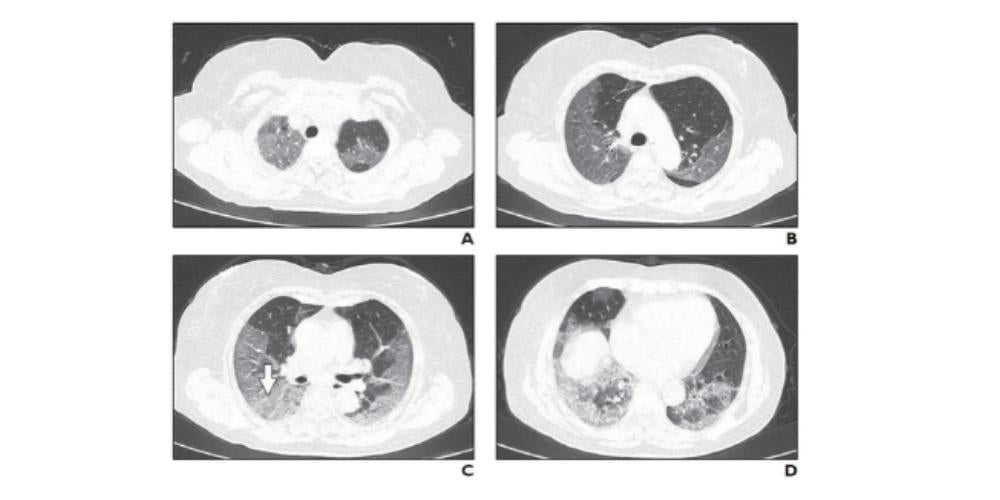
- COVID-19 pneumonia’s appearance is usually ground-glass opacities or peripheral consolidation on chest x-ray and CT
- CT is accurate and should be trusted, regardless of whether the polymerase chain reaction (PCR) test is negative. Consider repeating the PCR test in these cases.
- To predict the clinical course, repeat the CT scan around day 7 if a previous CT is available.
- Do not forget that patients may have pathologies other than COVID-19
Dr. Stephan Achenbach, an expert on cardiac imaging and chair of the department of cardiology at Friedrich-Alexander-Universität Erlangen-Nürnberg in Germany, moderated the ESC webinar. He noted that PCR remains the initial screening test for patients, but that medical imaging is used when symptoms are present. For sick patients, a CT result which points to COVID-19 signifies that patients can be sent directly to the hospital without waiting for the PCR result.
Both experts, Achenbach and Khalil, noted that medical imaging is a good predictor of clinical course. Evolution is persistent in COVID-19 cases and a worsening of lung abnormalities can help physicians predict that a patient’s condition is declining.
Khalil added that, “the extent of parenchymal lesions correlates with oxygen requirements. This extent also predicts the evolution towards resuscitation and mechanical ventilation."
For example, a patient with visible ground-glass opacities on CT or x-ray and who requires no oxygen at day 3 may display an extension of ground-glass opacities. By day 9, the patient could require oxygen, and by day 13 be experiencing respiratory distress and require hospitalization.
Depending on when patients experienced COVID-19 related symptoms and their first examination, Khalil recommended that physicians perform a CT scan at day 7 and again at day 15. He went on to note how further CT scans should be performed in according with the patient’s evolution and need for oxygen.
However, there are other physicians on the front lines of the COVID-19 pandemic who differ in their opinion on which medical imaging technique is most adept for diagnosis and treatment. Doctor Volpicelli stressed how he and his team had developed a method to diagnose and exam suspected or confirmed COVID-19 patients in Turin, Italy by relying on lung ultrasound.
Watch the webinar below: